Leakage, delays, and manual reviews are costing you.
2M claims vetted. $100M+ in claim value processed. $15M+ saved.
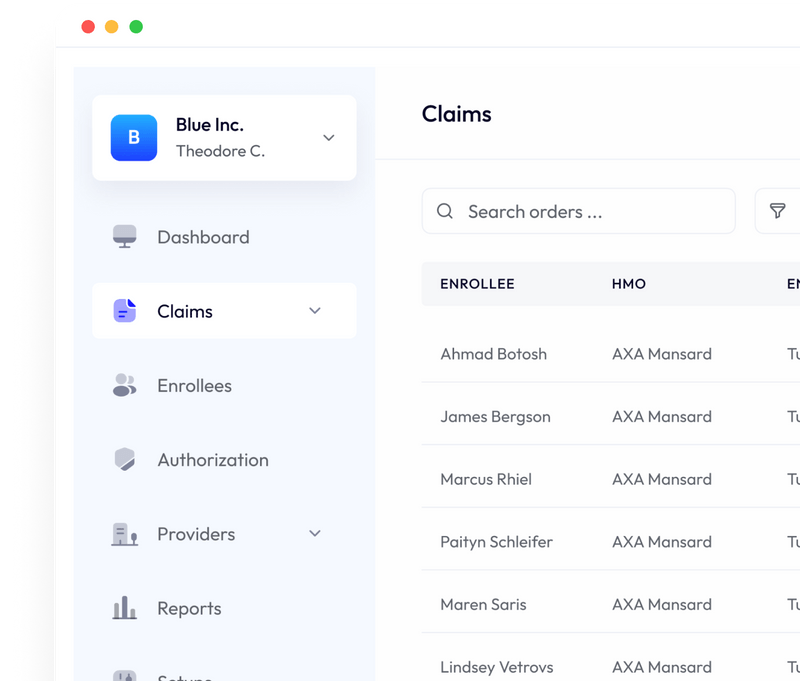
Curacel is the AI-powered claims platform trusted by insurers across Africa.
Curacel helps insurers and HMOs improve turnaround time, tighten controls, and reduce leakage — without slowing down approvals.
By the numbers (2025)

2M Claims Vetted
Operational scale you can trust

$100M+ Claims Value Processed
High Volume processing with control
99% Completion Rate
Increased completion rate across Auto AI-powered channels

$15m+ Saved
Prevented losses through smarter vetting &process controls
Built for teams managing claims at scale:
- Health insurers & HMOs (claims, medical, ops teams)
- Leaders tightening preauth controls and reducing leakage
- Teams needing faster turnaround with auditability and compliance
How it Works (20 mins)
- Share your current workflow — claims, preauth, deductions, exceptions
- We identify quick wins — controls, leakage points, automation opportunities
- You get a recommended rollout — what to automate first + expected impact
Trusted by teams that care about outcomes

FAQs
We've compiled a list of common questions to help you get the most out of Curacel
Can't find what you're looking for?
No — but enterprise teams see the fastest ROI due to claim volume and process complexity.
A quick overview of your claims workflow, approval process, and top recurring vetting reasons.
Yes — we support teams across Africa and beyond, with workflows tailored to local requirements.
Typically yes. During the review, we'll recommend the lightest integration path for your setup.
Want outcomes like this in 2026?
Book a 20-min workflow review and we'll show where savings and control improvements are most likely in your process.