Safe AI for Health Claims: The Curacel Blueprint for Profitable Automation
Most health claims operations are a patchwork of legacy systems, email inboxes, and spreadsheets. That’s a mess that costs money and frustrates providers. While Artificial Intelligence (AI) promises speed, fraud detection, and efficiency, integrating it safely is critical.
This guide provides a minimal, secure IT architecture — a blueprint that allows you to safely plug AI into your existing systems. It focuses on clarity, compliance, and driving revenue by reducing leakage. Curacel provides the end-to-end infrastructure to make this vision a reality, turning chaotic manual work into automated excellence.
If you’re wondering how claims evolved to this digital point, check out this history of claims management for context on where AI fits into modern processing.
The Claims System Blueprint: Six Cohesive Steps
You don't need a massive system overhaul. The Curacel approach treats AI and automation as intelligent layers, connecting your existing core systems into a predictable, efficient flow.
1. Intake: The Digital Front Door

This is where claims and documents arrive; from provider portals, APIs, or EDI. Your system needs to perform basic checks (member eligibility, dates) right away.
Curacel's tools integrate seamlessly to unify these entry points, immediately establishing a single source of truth for all incoming claims data.
For non-technical team members, this easy guide to health claims management explains the whole flow simply.
2. Data Preparation: Making Sense of Messy Files
The key to automation is transforming invoices, scans, and reports into structured, usable data. This requires Optical Character Recognition (OCR) and Curacel's quality gates to ensure documents are legible and all key totals are present.
3. Rules Engine: Consistent Decisions
This layer applies your clear business logic: coverage validation, benefit limits, and prior authorization checks. Anything that requires human review is tagged with a clear reason code (e.g., "limit exceeded").
4. AI Services: The Smart Investigator

AI should provide extra signals, not secret decisions. Curacel's AI-powered Claims Detection identifies duplicates, anomalies, and potential upcoding or fraud patterns up to 12x better than manual systems, providing adjusters with a clear summary of oddities. This reduces payouts on fraudulent claims by approximately 25%.
5. Decisioning & Routing: Straight-Through Processing (STP)
This is the profit driver. If the claim passes all rules and AI checks, it moves instantly to payment (STP). If not, it routes to the right human handler with the full digital evidence package. Curacel's platform is built to maximize STP, accelerating cash flow and improving provider satisfaction.
6. Payments & Reconciliation: The Financial Close
The final step is rapid disbursement and closing the financial loop. Your system must match the payout back to the original claim ID and archive every step for audit.
🔒 Non-Negotiable Guardrails: Safe and Compliant AI
To win stakeholder trust, especially in Legal and IT, your AI setup must be secure. Curacel ensures your integration meets stringent security standards:
- Data Security: Data is protected with encryption everywhere (in transit and at rest) and strict least-privilege access controls.

- Human-in-the-Loop: Any adverse decision (decline, fraud referral) must be reviewable by a person, with the full evidence the AI used—never black-box.
- Audit-Ready: Every AI signal, rule decision, and payment action is logged with a timestamp (Observability).
For executives needing a clear ROI, a broader digital claims explainer covers why real-time checks, automation, and analytics are crucial for reducing leakage and increasing speed.
Phase-Based Rollout: Achieve ROI with Low Risk
Curacel recommends a gradual, measurable adoption to prove value before expanding.
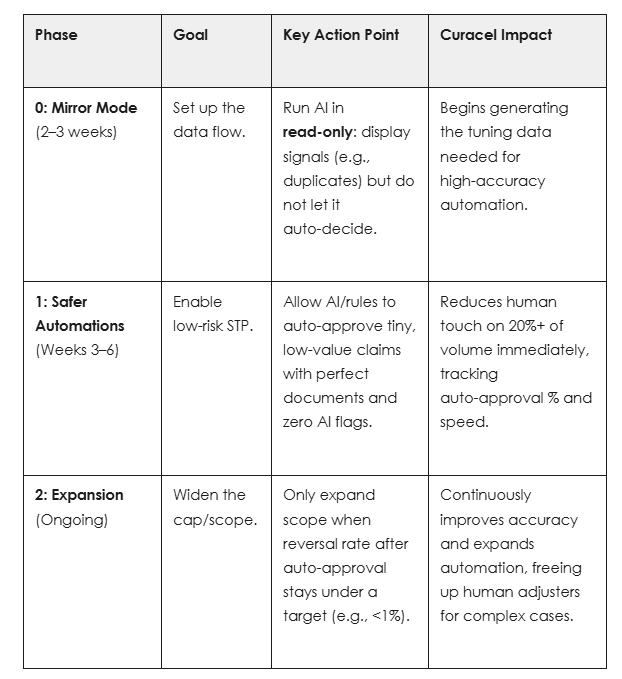
The result: fewer manual handoffs, reduced payment leakage, and faster settlements.
Ready to transform your health claims process and gain 70%+ efficiency?
Stop letting manual steps slow down your business. It's time to leverage AI built for the complexity of insurance.
Book your discovery call today and let us map your guaranteed path to Curacel claims automation.
Subsribe to our newsletter to receive weekly content























.svg)





