The Ultimate Guide to Automating Insurance Claims and Boosting Efficiency
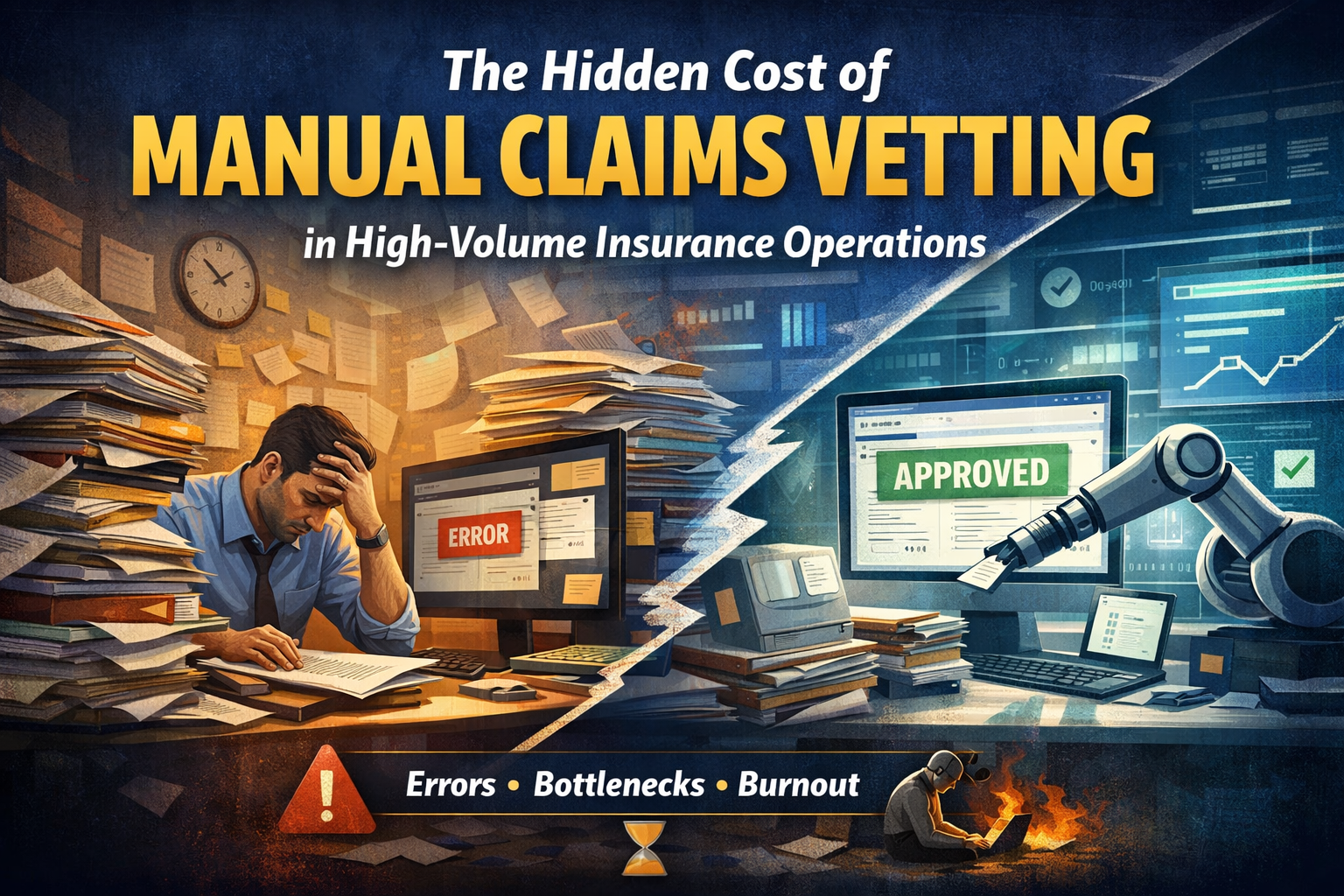
Manual claims processing is a bottleneck most insurers can't afford. Rising claim volumes, customer expectations for faster payouts, and thin margins make the old way—paper trails, manual reviews, endless queues—unsustainable.
Claims automation changes the equation. It's not about replacing your team; it's about freeing them from repetitive tasks so they can focus on decisions that actually need human judgment.
Book a 20-minute consultation →
What Is Insurance Claims Automation?

Key Components
- Document capture & extraction — Automatically pull data from invoices, medical reports, and photos
- Eligibility verification — Instantly confirm coverage, limits, and policy terms
- Rules-based adjudication — Apply policy logic consistently across all claims
- Exception routing — Flag complex cases for human review
- Payment processing — Automate settlement for approved claims
- Audit trail generation — Document every decision for compliance
Where AI Fits In
AI takes automation beyond digitisation. Instead of just moving paperwork electronically, AI-powered systems actually process claims—recognising patterns, flagging anomalies, and learning from historical data to improve over time.
How Automating Claims Boosts Efficiency
The impact shows up across four dimensions:
Speed
- Claims that took days now resolve in hours
- Straight-through processing (STP) handles routine claims without manual intervention

Accuracy
- Automated rules don't get tired or distracted
- Consistent policy application reduces errors, denials, and appeals
Cost
- Fewer manual touchpoints = lower cost per claim
- Handle higher volumes without proportional headcount increases
Experience
- Faster, more accurate claims = happier customers and providers
- Retention and reputation you can measure
McKinsey's research confirms that insurers redesigning claims with automation see significant improvements in both cost and customer satisfaction.
The Role of AI in Claims Automation
AI isn't a buzzword—it's the difference between digitisation and transformation.
Intake & Validation
- Extract data from documents automatically
- Check completeness without manual review
- Eliminate data entry and chasing missing information
Adjudication
- Apply policy rules via machine learning models
- Verify eligibility and approve routine claims instantly
- Route complex cases to the right specialist with full context
Fraud Detection
- Spot anomalies humans miss
- Flag unusual billing patterns and duplicate claims
- Detect provider behaviour that deviates from norms
Learn how Curacel powers insurance claims automation with built-in fraud controls.
Decision Consistency
- Every claim evaluated against the same logic
- Audit trails that satisfy regulators
- Reduced compliance risk
Benefits of Automating the Claims Process

Reduced Human Error
Eliminates typos, miscalculations, and inconsistent rule application that plague manual processes.
Enhanced Fraud Detection
AI catches suspicious claims before payout—not after.
Scalability
Handle 3x the volume without 3x the headcount. Automation absorbs growth while your team focuses on high-value work.
Compliance Confidence
Automated audit trails document every decision, making regulatory reviews straightforward.
Lower Operational Overhead
Less rework, fewer appeals, faster cycle times—all translating to hard cost savings.
To see real-world results from our clients, the numbers tell the story.
Claims Automation Software: What to Look For
Not all platforms deliver equal value. Prioritise these capabilities:
Must-Have Features
- AI-powered processing — Intelligent document extraction, rules-based adjudication, anomaly detection
- Configurability — Adjust business rules without developer dependency
- Integration — Connects to core admin systems, provider networks, payment rails
- Explainability — Reviewers see why claims are flagged or denied
- Reporting — Tracks STP rate, TAT, cost per claim, leakage—not vanity metrics
How to Implement Claims Automation
A phased approach reduces risk and builds momentum.
Step 1: Assess Your Current Process
- Map your claims journey end-to-end
- Identify bottlenecks, errors, and leakage points
- Establish your baseline metrics
Step 2: Choose the Right Platform
- Match capabilities to your specific pain points
- Prioritise quick wins (intake automation) before complex adjudication
Step 3: Integrate with Existing Systems
- Work with vendors that support your tech stack
- Avoid platforms requiring core infrastructure replacement
Step 4: Train Your Team
- Automation changes roles, not eliminates them
- Invest in training so staff work with the system
Step 5: Monitor & Optimise
- Track KPIs from day one
- Use data to refine rules and expand automation coverage
Overcoming Common Challenges
Resistance to Change
Solution: Involve operations teams early. Show them automation handles tedious work—freeing them for more interesting problems.
Integration Complexity
Solution: Choose platforms with modern APIs and proven integrations. Avoid custom builds where possible.
Compliance Concerns
Solution: Ensure full audit trails and explainable decisions. Regulators want transparency, not black boxes.
Data Quality Issues
Solution: Use implementation as an opportunity to clean up. Better data means better outcomes.
Claims Automation in Action
Insurers using Curacel's platform have achieved:
- ✅ Faster turnaround times
- ✅ Reduced leakage
- ✅ Scaled claims volume without proportional headcount growth
How Curacel's claims automation solution improved claims processing shows outcomes across health and motor insurance deployments.
Ready to Automate?
Claims automation isn't optional anymore—it's how modern insurers compete. The question isn't whether to automate, but where to start.
We can help you:
- Map your claims journey
- Identify quick wins
- Build a business case that gets executive buy-in
Book a 20-minute consultation →
Abonnez-vous à notre newsletter pour recevoir du contenu hebdomadaire
























.svg)







