Claims Management: Taking a Determined Stand Against Insurance Fraud
Insurance fraud is a deliberate deception perpetrated against or by an insurance company or agent for financial gain.
Fraud is an increasing challenge, and combating fraud has a considerable cost on insurers.
Insurance Fraud may be committed at different points in the transaction by applicants, policyholders, third-party claimants, or professionals who provide services to claimants. Insurance agents and company employees are sometimes involved in committing insurance fraud.
Common insurance frauds include:
- Padding or inflating claims
- Misrepresenting facts on an insurance application
- Submitting claims for injuries or damage that never occurred
- And staging accidents
Healthcare and auto insurance are considered to be two of the most affected sectors.
Auto insurance fraud
Auto insurance fraud spans from misrepresenting facts on insurance applications and inflating insurance claims to staging accidents and submitting claim forms for injuries or damage that never happened, to false reports of stolen vehicles.
Fraud accounted for between 15% to 17% of total claims payments for auto insurance in 2012, according to an Insurance Research Council (IRC) study. The study also estimated that between $5.6 billion and $7.7 billion was fraudulently added to paid claims for auto insurance bodily injury payments in 2012, compared with a range of $4.3 billion to $5.8 billion in 2002.
Healthcare fraud
Healthcare fraud affects all types of property/casualty insurance coverage that include a medical care component, such as medical payments for auto accident victims or workers injured in the workplace or an individual who needed a medical check-up.
Fraud, waste and abuse (FWA) occur at many points in the healthcare system - doctors, hospitals, nursing homes, diagnostic facilities and medical equipment suppliers - have all been mentioned to defraud the system.
It's been reported that the financial losses due to health care fraud are in the tens of billions of dollars each year.
The most prevalent types of healthcare fraud are:
- Billing for services not rendered
- Upcoding services and medical items (where the provider submits a bill using a code that yields a higher payment than for the service or item that was rendered)
- Filing duplicate claims
- Unbundling (billing in a fragmented fashion for tests or procedures that are required to be billed together at reduced cost)
- Performing excessive services
- Performing unnecessary services
- And offering kickbacks
Health insurance and medical fraud have a particularly large financial impact.
And health-related fraud increased during the COVID-19 pandemic.
The cost of insurance fraud
“Many people think insurance fraud is a “victimless crime” where the only ones who lose are the insurance companies and their executives with deep pockets. However, this could not be further from the truth,” according to Insurance Business.
Studies suggest that a section of insurance fraud committed by consumers is driven by revenge or retaliation for a personal service exchange which they think is unfair. People may retaliate to “get a return” or “get their money’s worth.”
Use of technology to combat fraud
One of the most effective means of combating insurance fraud is the adoption of data technologies that cut the time needed to recognize fraud.
Progress in analytical technology is crucial in combating fraud to keep pace with sophisticated and new tactics constantly developed by scammers.
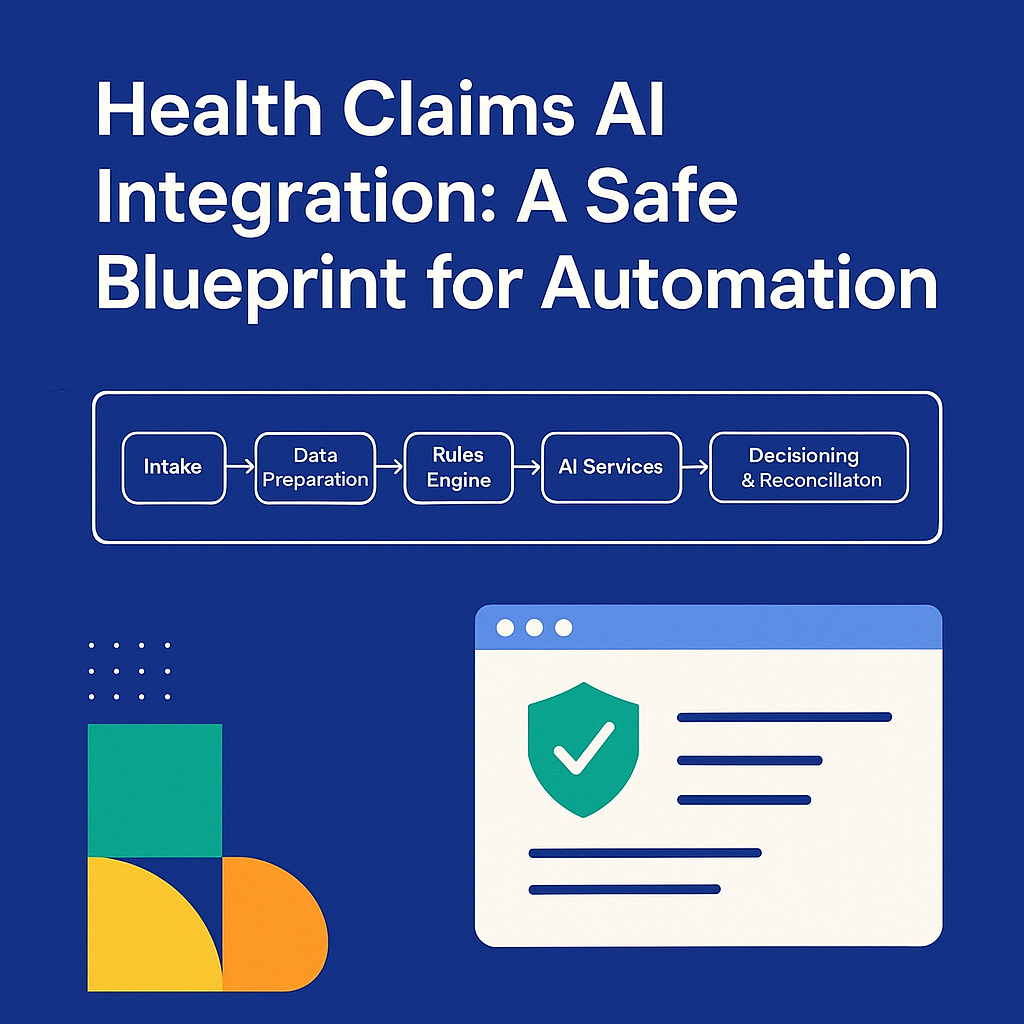
Artificial intelligence, among other tech tools, can be used to uncover fraud in claims processing before a payment is made. These strategies are employed when claims are first filed.
Suspicious claims are flagged for further review, while those with no suspicious elements are processed normally.
In search of refinement, insurers are blending tools to improve their fraud detection programs.
Using Curacel Claims Automation
Curacel Claims Automation is a cutting-edge AI solution. Curacel powers claim management and processing by making predictions, optimizing claims' outcomes, and flagging suspicious claims and potential fraud resulting in enhanced process efficiency and customer experience.
Find out more about how you can manage your claim management and processing with Curacel Claims.
Subsribe to our newsletter to receive weekly content

























.svg)







